Measles Resurgence: Why Cases Are Rising and What to Do?
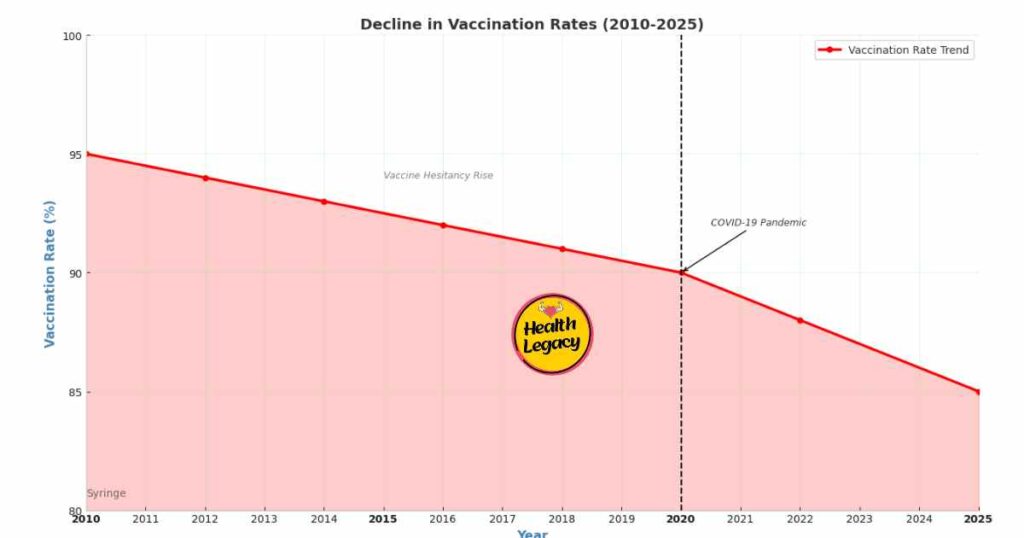
In 2025, the United States is witnessing a troubling measles resurgence, with cases surging in states like Texas, Kansas, and Colorado. Once declared eliminated in 2000, measles—a highly contagious infectious disease—is making a comeback, driven by declining vaccination rates and weakening herd immunity. The MMR vaccine, a cornerstone of public health, has kept this disease at bay for decades, but its effectiveness relies on widespread use. Today, with vaccination rates dipping below the critical 95% needed for herd immunity, experts warn of a growing threat to child health and community safety.
This article explores the causes of the measles resurgence, the science behind vaccination, and the strategies needed for outbreak prevention. From vaccine hesitancy to health policy, we’ll examine the factors at play and offer insights into protecting future generations.
The History of Measles and Vaccination Success
Measles has a long, grim history. Before the 1960s, it infected millions annually in the U.S., causing fevers, rashes, and, in severe cases, death. The introduction of the measles vaccine in 1963, followed by the MMR vaccine in 1971, transformed public health. By combining protection against measles, mumps, and rubella, the MMR vaccine slashed cases dramatically. By 2000, the U.S. declared measles eliminated—a testament to high vaccination rates and robust health policy.
Also Read : What’s Behind the Autism Registry? RFK Jr. Explained
This success wasn’t accidental. It stemmed from coordinated efforts to ensure child health through widespread vaccination. Yet, elimination isn’t eradication. Measles persists globally, and the U.S. depends on herd immunity to keep it out. Recent declines in vaccination rates have jeopardized this shield, fueling the measles resurgence.
The Current Measles Resurgence: A Snapshot
Today, the measles resurgence is undeniable. In the first quarter of 2025, over 300 cases were reported nationwide, far exceeding recent years. Texas saw a tragic milestone: the first measles-related death in over two decades—an unvaccinated child. National vaccination rates for the MMR vaccine have slipped to 91%, below the 95% threshold for herd immunity. In some communities, rates are even lower, creating vulnerable pockets where this infectious disease thrives.
Herd immunity is the backbone of outbreak prevention. When 95% of a population is vaccinated, measles struggles to spread, protecting even those who can’t be immunized, like infants or the immunocompromised. Falling below this mark, as we are now, invites outbreaks—putting child health and public health at risk.
Why Are Vaccination Rates Declining?
The drop in vaccination rates isn’t random. Several factors are driving this trend:
- Vaccine hesitancy: Misinformation, such as the debunked claim linking vaccines to autism, fuels distrust. Despite decades of research proving MMR vaccine safety, myths persist online and in communities.
- Pandemic disruptions: COVID-19 halted routine vaccination schedules, leaving many children unprotected. Some families have yet to catch up.
- Access barriers: Rural and underserved areas lack easy access to vaccination services, a challenge seen from Texas plains to global regions like rural India.
- Complacency: With measles rare for years, some parents see less urgency in vaccination, underestimating its risks.
These issues have converged, weakening herd immunity and sparking the measles resurgence.
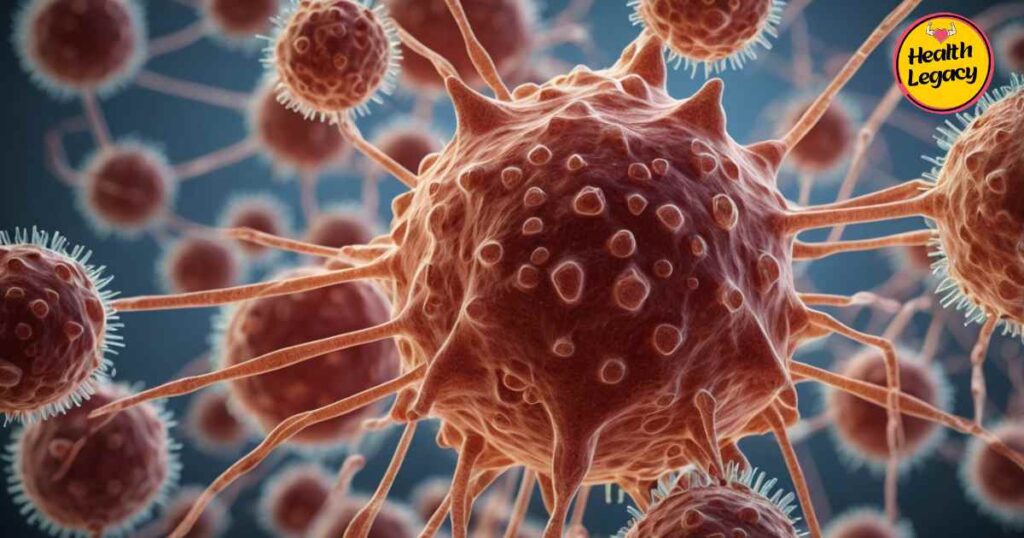
The Science Behind Measles and the MMR Vaccine
Measles is a powerhouse of contagion. Spread through respiratory droplets, it can linger in the air for hours. Symptoms—fever, cough, red eyes, and a rash—emerge 10-14 days after exposure. While many recover, complications like pneumonia or encephalitis can be fatal, especially for unvaccinated kids.
Also Read : Top 10 Best Holistic Health Practices for Well-Being
The MMR vaccine is a proven shield. With two doses (at 12-15 months and 4-6 years), it’s 97% effective. It uses weakened viruses to train the immune system without causing illness. Extensive studies confirm its safety—no link to autism or other serious risks exists. Beyond individual protection, it bolsters herd immunity, a key pillar of public health.
Case Studies: Measles Outbreaks Up Close
Real-world examples reveal the toll of the measles resurgence:
- Texas, 2025: In a town with vaccination rates at 85%, an unvaccinated child returned from abroad with measles. The outbreak infected 170 people, including a 3-year-old who died from pneumonia. It exposed gaps in herd immunity and strained local public health resources.
- Colorado Suburb: Here, vaccine hesitancy thrived, fueled by local misinformation. An outbreak hit, sickening 50 and hospitalizing several. Attitudes shifted only after a community leader fell ill, prompting a slow rise in vaccination rates.

These cases underscore the stakes: without strong vaccination efforts, child health suffers, and outbreaks spiral.
Public Health Strategies for Outbreak Prevention
Stopping the measles resurgence demands action:
- School mandates: States with strict vaccination requirements see higher vaccination rates. Reducing exemptions can close gaps.
- Community outreach: Mobile clinics and partnerships with local leaders can boost access and trust in underserved areas.
- Education: Campaigns debunking myths about MMR vaccine safety are vital. Resources like those from the CDC or WHO can empower parents.
- Healthcare roles: Doctors can address vaccine hesitancy, ensuring kids stay on track with MMR vaccine schedules.

These health policy measures can rebuild herd immunity and protect public health.
The Global Measles Challenge
The measles resurgence isn’t unique to the U.S. Globally, 107,500 died from measles in 2023, mostly in nations with low vaccination rates. Countries like Nigeria and India battle high case loads due to limited healthcare access. The U.S., at 91% coverage, ranks better but lags behind leaders like Sweden (97%).

International travel adds risk—unvaccinated Americans can import measles, igniting outbreaks. Global initiatives, like the WHO’s Measles & Rubella Partnership, offer lessons in outbreak prevention that could strengthen U.S. health policy.
Also Read : Mindfulness Techniques for Beginners: Your Guide to Calm and Clarity 2025
Socioeconomic Factors in Vaccination Disparities
The measles resurgence hits harder in certain groups. Low-income families often face barriers to vaccination—fewer clinics, transportation issues, or time off work. Education levels also matter; higher education correlates with lower vaccine hesitancy. Cultural beliefs, too, shape attitudes—some communities resist vaccination on religious grounds.

Data shows stark contrasts: urban areas with robust public health infrastructure often exceed 95% vaccination rates, while rural counties dip below 80%. Addressing these disparities is key to restoring herd immunity and safeguarding child health.
The Role of Technology in Measles Control
Innovation could turn the tide on the measles resurgence. New tools include:
- Vaccine delivery: Microneedle patches could simplify MMR vaccine administration, especially in remote areas.
- Digital tracking: Apps or health records can send vaccination reminders, reducing missed doses.
- Misinformation countermeasures: AI-driven platforms can flag false claims about MMR vaccine safety, supporting public health efforts.
These advances, paired with strong health policy, could enhance outbreak prevention and boost vaccination rates.
Future Scenarios: Where Are We Headed?
The future of measles in the U.S. hinges on vaccination rates. If they stagnate below 95%, the measles resurgence could worsen, with larger outbreaks threatening herd immunity. Measles might even become endemic again—a step backward for public health.

But optimism isn’t lost. If health policy strengthens, vaccine hesitancy fades, and access improves, we could reclaim control. Projections suggest a 5% rise in vaccination rates could halve cases by 2030. The path forward depends on collective action.
Also Read : Transform Your Gut Health with These 7 Probiotic Diet Hacks!
Recommendations for Stakeholders
To combat the measles resurgence, everyone has a role:
- Parents: Ensure kids get the MMR vaccine on time. Consult pediatricians to address vaccine hesitancy.
- Policymakers: Fund public health initiatives and enforce vaccination mandates.
- Healthcare providers: Educate families on MMR vaccine benefits and infectious disease risks.
- Communities: Promote vaccination drives to protect child health.
These steps can rebuild herd immunity and halt outbreaks.
FAQs
What are the early signs and symptoms of measles in children?
Early signs of measles in children include high fever, cough, runny nose, and red, watery eyes. A rash appears days later, starting on the face and spreading to the body.
How effective is the MMR vaccine in preventing measles infections?
The MMR vaccine is highly effective, offering 97% protection against measles infections with two doses, making it vital for community immunity.
What is herd immunity and why is it important for preventing measles outbreaks?
Herd immunity occurs when 95% of people are vaccinated, limiting measles spread and protecting those who can’t be vaccinated from outbreaks.
Why are childhood vaccination rates declining in the United States?
Childhood vaccination rates are dropping due to vaccine hesitancy, misinformation about safety, and disruptions from the pandemic.
What are the potential health complications of measles in unvaccinated children?
Measles in unvaccinated children can lead to pneumonia, encephalitis, and death, underscoring the need for vaccination.
How can parents protect their children from measles during an outbreak?
Parents can safeguard kids with timely MMR vaccine doses, avoiding sick individuals, and adhering to outbreak health protocols.
How does the measles resurgence in the U.S. compare to global trends?
The U.S. measles resurgence ties to declining vaccination rates, while globally, cases soar in areas with poor healthcare access.
Conclusion: A Call to Action
The measles resurgence is a wake-up call. Declining vaccination rates have weakened herd immunity, endangering child health and public health. The MMR vaccine remains our best tool, but it works only if we use it. By tackling vaccine hesitancy, improving access, and strengthening health policy, we can stop measles in its tracks.
Check your family’s vaccination status today. Support outbreak prevention efforts in your community. Together, we can protect the next generation from this preventable infectious disease.